Maternal Health in Louisiana
Maternal health outcomes help assess the overall well-being of communities. In the United States, where the maternal mortality rate is the highest among all developed countries, the deaths of mothers happen far too often. The Louisiana Pregnancy-Associated Mortality Review (PAMR) Committee works to understand pregnancy-associated deaths through epidemiological surveillance and multidisciplinary case review. A pregnancy-associated death is defined as a death that occurs during pregnancy or within one year of the end of pregnancy, regardless of the cause. The purpose of this review is to bring awareness to this public health issue and to create actionable recommendations to prevent future deaths. The latest report and supplemental materials can be found below.
Most Recent PAMR Report & Materials
What Do We Know?
Maternal deaths are not isolated events. We cannot fully understand disparities in maternal health outcomes without understanding the role of health inequities. Systemic issues such as racism and implicit biases impact our environmental conditions, sources of social support, economic security, and the quality of care we receive. All of these are social factors important for living healthy lives. Placing health equity at the center of all work combatting maternal mortality helps us improve health outcomes for everyone.
Important PAMR Data Highlights
- There were 82 pregnancy-associated deaths identified in 2020. The majority of deaths (78%) were pregnancy-associated, but not related to the pregnancy. 15 deaths (18%) were pregnancy-related.
- The top causes of pregnancy-associated, but not related deaths were accidental overdose, homicide, motor vehicle collision, and cancer.
- The top causes of pregnancy-related deaths were cardiomyopathy, accidental overdose, infection, and cardiovascular conditionss.
- Racial disparities exist. 37% of all births in Louisiana in 2020 were to non-Hispanic Black women, but non-Hispanic Black women accounted for 62% of all pregnancy-associated deaths.
- 13 out of 15 pregnancy-related deaths occurred among Black women.
- Most deaths occurred after delivery up to 1-year after pregnancy. The majority of all deaths, 93% of pregnancy-related and 71% of pregnancy-associated, but not related, occurred after delivery up to 1 year after pregnancy.
- Many deaths were potentially preventable. The committee determined that 94% of pregnancy-related deaths and 80% of pregnancy-associated, but not related deaths were potentially preventable.
What Can Be Done?
Maternal mortality affects everyone. Each death represents a life lost, a family changed. Eliminating these outcomes will take all of us. Together, using our roles as individuals, family members, healthcare providers, and policymakers, we can create solutions and help our Louisiana communities thrive.
Get involved with some recommendations for prevention led by the Bureau of Family Health:
- Improving care coordination before, during, and after pregnancy. Providers can refer patients to the Maternal, Infant, and Early Childhood Home Visiting program (MIECHV). This program connects families with personalized support and coaching from nurses and parent educators.
- Improving the identification and treatment for substance use and mental health conditions during pregnancy. The Provider to Provider Consultation Line (PPCL) provides a no-cost mental health consultation line to providers working with pregnant and postpartum patients. Give them a call at 504-988-9171.
- Ensuring pregnant people receive the appropriate level of care. Birthing facilities can work with the Louisiana Perinatal Quality Collaborative (LaPQC) on improving birth outcomes through work such as the Safe Births Initiative. Contact LaPQC@la.gov to learn how you can contribute.
About Pregnancy-Associated Mortality Review
In 2010, the Louisiana Pregnancy-Associated Mortality Review (PAMR) program was established by the Louisiana Department of Health’s Office of Public Health’s Bureau of Family Health to understand and address maternal mortality in our state.
In 2018, Louisiana PAMR launched an enhanced multidisciplinary review process to be in full alignment with national best practices promoted by the CDC. Louisiana’s PAMR work is funded by the CDC’s Enhancing Reviews and Surveillance to Eliminate Maternal Mortality (ERASE-MM) program, and is authorized by the Louisiana Commission on Perinatal Care and Prevention of Infant Mortality (Louisiana Perinatal Commission). Louisiana PAMR works to quantify and understand pregnancy-associated deaths in order to create actionable, comprehensive recommendations to prevent future deaths. We do this through epidemiological surveillance and multidisciplinary case review of all pregnancy-associated deaths, which is the death of an individual while pregnant or within one year of the end of pregnancy, regardless of the cause of death.
The case review process was further enhanced by expanding the PAMR committee to ensure representation from a variety of geographic regions and fields of expertise, including substance use and mental health. The Louisiana PAMR committee prides itself in its diversity of disciplines as well as gender, race, and ethnicity. Today, the committee consists of both clinical and non-clinical experts. To ensure that the committee’s work is informed by individuals who know and understand the context of Louisiana, the Bureau of Family Health team continues statewide recruitment efforts. In 2023, we enhanced our recruitment process, seeking member with diverse perspectives on maternal health, by launching a statewide application open to healthcare professionals, community health/public health workers, community-based organizations, social services, community advocates, individuals with expertise in racism, discrimination, and health equity, and individuals with lived experience as members of communities disproportionately impacted by maternal mortality.
Louisiana PAMR’s mission is to protect and promote the health of women and families in Louisiana through surveillance, multidisciplinary case review, timely reports, and provision of actionable recommendations. This helps to understand and prevent pregnancy-associated deaths and support prevention, transformation, and innovation in individuals, families, providers, birthing facilities, health systems, and communities.
Louisiana PAMR’s goals are to:
- Perform a multidisciplinary review of cases to gain a holistic understanding of the issues
- Determine the annual number of maternal deaths related to pregnancy
- Identify trends and risk factors among pregnancy-associated deaths in Louisiana
- Recommend improvements to care at the individual, provider, and system levels with the potential for reducing or preventing future events
- Prioritize findings and recommendations to guide the development of preventive measures
- Recommend actionable strategies for prevention and intervention
- Disseminate the findings and recommendations to a broad array of individuals and organizations
- Promote the translation of findings and recommendations into quality improvement actions at all levels
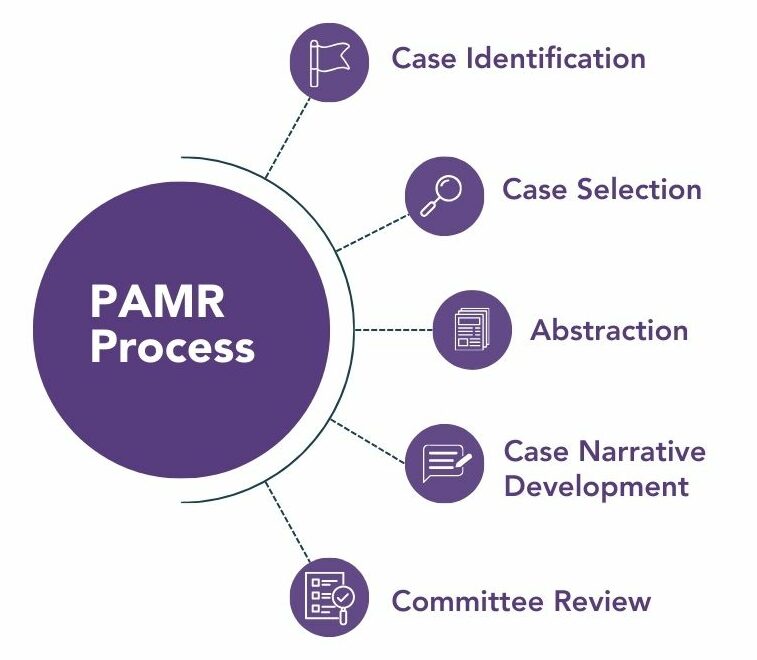 Deaths are identified through a combination of linkages, the pregnancy checkbox on death certificates and obstetric code (O-code) causes of death. Deaths are identified in four steps:
Deaths are identified through a combination of linkages, the pregnancy checkbox on death certificates and obstetric code (O-code) causes of death. Deaths are identified in four steps:
- Data linkages: Death certificates of women between the ages of 10-55 are linked to infant birth and fetal death certificates that occurred within one year using SAS in conjunction with the LinkPro macro and Link King to complete all linkages.
- Pregnancy checkbox: Death certificates with the pregnancy checkbox filled in, indicating the decedent was pregnant at the time of death or within one year of pregnancy, are identified as potential pregnancy-associated deaths.
- O-codes: Deaths of women where the ICD-10 code for underlying cause of death is in chapter
O (causes related to pregnancy, childbirth or complications during the postpartum period) are identified as potential pregnancy-associated deaths. - LaHIDD linkages: Linkages between death records and hospital discharge records are conducted to identify additional cases. All women between the ages of 10 and 55 who had any pregnancy-related ICD-10CM codes are included. Women who were found to have a delivery, positive pregnancy test or an ectopic pregnancy are identified as potential pregnancy-associated deaths. LaHIDD linkages are conducted using Link Plus and Link King software.
CASE VALIDATION AND CONFIRMATION (SELECTION)
Because of data limitations, the use of vital records death data and data linkages alone is not enough to identify true pregnancy-associated deaths. Potential pregnancy-associated deaths identified using the above mentioned methods require validation by the Bureau of Family Health’s Maternal and Child Health (MCH) Coordinators using medical records and/or coroner reports. This validation process reduces or eliminates “false positive” identifications of pregnancy-associated deaths that could result from the pregnancy box being checked in error, errors in ICD-10 codes, or when a birth and death record are incorrectly identified as a match. A death is considered “confirmed”, and therefore eligible for review, if the MCH Coordinator confirms a pregnancy within one year of death based on the available records.
CASE ABSTRACTION AND CASE NARRATIVE DEVELOPMENT
Once a case is confirmed as a pregnancy-associated death, the regional MCH Coordinators abstract data from various sources including, but not limited to, prenatal/postpartum care, hospital, behavioral health, coroner, EMS, and law enforcement records. Using information obtained during the abstraction process, the MCH Coordinators develop a de-identified case narrative that details the decedent’s life from pre-conception through death, including both medical and social information.
CASE REVIEW AND DISCUSSION
The de-identified case narratives are sent to PAMR Committee members ahead of review meetings.
During meetings, the committee conducts an in-depth review of each case to determine if the death was pregnancy-related, if the death was preventable, what factors contributed to the death, and what, if any actions might have altered the course of events. The committee uses this knowledge to create specific, feasible recommendations for prevention. Recommendations are made at the levels of healthcare providers, healthcare systems, hospitals and birthing facilities, insurance payors, government and public health agencies, policy makers, and social local community organizations.
Throughout case discussions, respect and justice for the decedent are maintained. Anyone with personal knowledge of a particular case is asked to recuse themselves from the review process so to not share details or anecdotal information beyond the information presented in the case narrative.
Across the country, maternal mortality review committees (MMRCs) have found it difficult to categorize accidental overdoses and suicides as pregnancy-related or pregnancy-associated, but not related when posed with the questions “Was the death pregnancy-related? If this person was not pregnant, would they have died?”
The Utah MMRC conducted a retrospective review of all pregnancy-associated and pregnancy-related deaths and found that “pregnancy itself was the inciting event leading to the majority of accidental drug-related deaths or suicides among pregnant and postpartum women.” After this study, they created a standardized tool to help other MMRCs determine pregnancy-relatedness for deaths due to accidental drug overdoses and suicides. This tool was shared with other state level MMRCs and has led to better identification of pregnancy-relatedness in the cases of accidental drug overdoses and suicides. Louisiana began using “The Utah Tool” in 2021 with the review of 2019 cases. Because of this, there has been a decrease in the number of cases that were classified as pregnancy-associated, but unable to determine relatedness.
Data shows that there are significant racial and ethnic disparities in pregnancy-associated mortality across the United States. In acknowledgement of these disparities and the importance of this issue, in 2020, the CDC asked MMRCs to determine whether or not discrimination contributed to the death during case reviews.
Disparity in maternal mortality is a complex issue that is due to many factors, including, but not limited to, implicit bias and structural racism impacting social determinants of health. With the data the committee has access to, determining racism, bias or discrimination as a contributing factor in a pregnancy-associated death can be difficult, but the Louisiana PAMR team is committed to reviewing each death through a lens of equity. To help the committee better answer the question “Did discrimination contribute to the death?” our team developed and began using the Louisiana Bias or Racism and Social Determinants of Health (LABoRS) Tool in 2020 with the review of 2018 cases.
The LABoRS Tool provides a standardized process to evaluate each case for the presence of bias, discrimination, and/or racism, as well as the impacts of social determinants of health as contributors to the death. The LABoRS Tool is not designed to prove bias and/or racism, but to assist abstractors as well as committee members in identifying evidence of potential discrimination and inequity. With the ability to identify potential bias and/or racism and social determinants of health, the PAMR committee is better able to make informed recommendations that address these contributing factors if they are present.
